Psychiatric nursing focuses on providing holistic care to individuals with mental health disorders, emphasizing empathy, scientific knowledge, and cultural competence to promote recovery and well-being.
1.1 Definition and Scope of Psychiatric Nursing
Psychiatric nursing, or mental health nursing, involves caring for individuals with mental health disorders. It encompasses assessment, diagnosis, and treatment of mental illnesses. The scope includes providing therapeutic interventions, education, and support to patients and their families. Psychiatric nurses work in various settings, such as hospitals, clinics, and community centers, promoting holistic care that addresses biological, psychological, social, and cultural aspects of mental health. Their role is vital in fostering recovery, well-being, and reintegration into society.
- Focuses on mental health disorders and emotional well-being.
- Integrates pharmacological and non-pharmacological interventions.
- Emphasizes patient-centered, holistic care approaches.
1.2 Historical Evolution of Psychiatric Nursing
Psychiatric nursing has evolved significantly from its origins in asylums during the Middle Ages to modern, patient-centered care. Early practices often lacked humanity, focusing on containment rather than treatment. The 18th and 19th centuries saw reforms, with figures like Dorothea Dix advocating for better conditions. The 20th century introduced psychotherapy and medications, shifting the focus to recovery. Today, psychiatric nursing emphasizes holistic, evidence-based care, respecting patients’ rights and dignity.
- Originated in asylums with poor conditions.
- Reforms in 18th-19th centuries improved care.
- 20th century advancements in therapy and medications.
- Modern focus on patient-centered, ethical practices.
1.3 Key Concepts and Principles
Psychiatric nursing is rooted in empathy, understanding, and therapeutic communication. Key principles include trauma-informed care, patient-centered approaches, and cultural competence. Nurses must establish trust, maintain boundaries, and prioritize confidentiality. Evidence-based practices guide interventions, ensuring safe and effective care. Self-awareness and emotional resilience are essential for nurses to manage stress and provide compassionate support. These principles foster a collaborative environment, empowering patients to achieve mental health recovery and improve their quality of life.
- Empathy and therapeutic communication.
- Trauma-informed and patient-centered care.
- Cultural competence and confidentiality.
- Self-care and emotional resilience.

Essential Skills for Psychiatric Nurses
Psychiatric nurses must master assessment, communication, and therapeutic interventions. Skills include empathy, active listening, and cultural competence to build trust and support patients’ mental health recovery effectively.
2.1 Assessment and Observation Techniques
Effective assessment and observation are critical in psychiatric nursing. Nurses use tools like mental status exams to evaluate patients’ cognitive, emotional, and behavioral states. Observing non-verbal cues, speech patterns, and mood shifts helps identify potential issues. Risk assessments for suicide or violence are also essential. Accurate documentation of findings ensures comprehensive care planning and continuity. These skills require attention to detail, empathy, and cultural sensitivity to provide individualized support while maintaining patient confidentiality and trust.
2;2 Communication Strategies with Patients
Effective communication is vital in psychiatric nursing. Active listening, empathy, and clear language help build trust and understanding. Nurses should adapt communication to the patient’s cognitive and emotional state, ensuring clarity and patience. Cultural competence is essential to address diverse beliefs and values. Non-verbal cues, such as eye contact and body language, also play a significant role. Open-ended questions encourage patients to express their feelings, fostering a therapeutic relationship and promoting collaborative care.
2.3 Therapeutic Interventions and Techniques
Therapeutic interventions in psychiatric nursing include evidence-based practices like cognitive-behavioral therapy (CBT), mindfulness, and psychoeducation. Nurses use de-escalation techniques to manage crises and promote a calm environment. Medication management and education are crucial to ensure adherence and effectiveness. Cultural sensitivity is key in tailoring interventions to individual needs. These techniques foster a collaborative therapeutic relationship, empowering patients to manage symptoms and improve their quality of life. Continuous assessment ensures interventions are adapted to meet evolving patient needs.

Legal and Ethical Considerations
Psychiatric nursing requires adherence to legal standards, patient rights, and ethical principles. Informed consent, confidentiality, and respect for autonomy are cornerstone practices, ensuring care is both lawful and compassionate.
3.1 Informed Consent and Patient Rights
Informed consent is a legal and ethical cornerstone in psychiatric nursing, ensuring patients understand and agree to their care. It must be voluntary, with patients fully aware of risks, benefits, and alternatives. Patient rights include autonomy, dignity, and confidentiality, with nurses advocating for these principles. Violations can lead to legal consequences, emphasizing the importance of adhering to ethical guidelines. These practices foster trust and ensure patient-centered, respectful care.
3.2 Confidentiality and Privacy in Care
Confidentiality and privacy are fundamental ethical and legal obligations in psychiatric nursing. Nurses must safeguard patients’ personal and medical information, adhering to laws like HIPAA. Patient records should be securely stored, and disclosures require explicit consent. Privacy respects patients’ dignity and fosters trust, crucial for therapeutic relationships. Breaches can lead to legal and ethical violations, underscoring the importance of rigorous confidentiality practices in all care settings.
3.3 Managing Challenging Behaviors
Managing challenging behaviors in psychiatric care requires a proactive approach. Nurses should identify triggers, use de-escalation techniques, and maintain a calm demeanor. Establishing clear boundaries and providing a safe environment helps reduce aggression. Documentation of incidents and interventions ensures accountability and informs future care strategies. Collaboration with multidisciplinary teams is essential to develop personalized plans, promoting patient safety and well-being while adhering to legal and ethical standards.
Safety in Psychiatric Care
Safety in psychiatric care prioritizes crisis intervention, de-escalation techniques, and risk assessments to prevent harm. Creating a secure environment ensures patient and staff well-being, fostering a safe space for recovery.
4.1 Crisis Intervention and De-escalation
Crisis intervention and de-escalation are critical skills in psychiatric nursing, focusing on managing volatile situations through active listening, empathy, and non-verbal communication. Nurses assess triggers, remain calm, and prioritize patient safety. Techniques include maintaining a safe distance, using open body language, and speaking in a soft tone. The goal is to prevent escalation, reducing the need for physical restraint. Effective de-escalation strategies ensure a safe environment for both patients and staff, fostering trust and cooperation during crises.
4.2 Risk Assessment and Prevention of Harm
Risk assessment in psychiatric nursing involves identifying potential dangers, such as self-harm or violence, to ensure patient and staff safety. Nurses use standardized tools to evaluate risk factors and develop tailored prevention strategies. Environmental modifications, close monitoring, and therapeutic interventions are key. Early detection of triggers and proactive measures minimize harm. Prioritizing patient safety while respecting dignity is essential. Effective risk management promotes a secure care environment, reducing adverse outcomes and fostering trust in the therapeutic relationship.
4.3 Safe Physical Environment Practices
Creating a safe physical environment in psychiatric care involves removing hazards, ensuring accessibility, and promoting comfort. Nurses should eliminate sharp objects, secure medications, and use furniture that minimizes injury risks. Calming colors, natural light, and noise reduction can reduce agitation. Regular environmental checks ensure safety and adaptability to patient needs. A well-designed space fosters a therapeutic atmosphere, enhancing patient well-being and reducing potential risks. Safety equipment, such as alarms, may be necessary in high-risk areas to protect both patients and staff.

Common Psychiatric Disorders
Psychiatric disorders include schizophrenia, mood disorders, anxiety disorders, PTSD, and eating disorders, each requiring tailored approaches for effective diagnosis and treatment in nursing care settings.
5.1 Schizophrenia and Psychotic Disorders
Schizophrenia is a chronic mental disorder characterized by hallucinations, delusions, disorganized thinking, and negative symptoms. Psychotic disorders involve disruptions in reality perception, often requiring specialized nursing interventions. Psychiatric nurses play a crucial role in assessing symptoms, providing emotional support, and educating patients and families about the condition. Treatment typically involves antipsychotic medications, combined with psychotherapy and lifestyle adjustments. Nurses must foster a therapeutic environment, promoting adherence to treatment plans and enhancing quality of life for individuals with these challenging conditions.
5.2 Mood Disorders: Depression and Bipolar Disorder
Mood disorders encompass a range of mental health conditions, primarily depression and bipolar disorder. Depression is marked by persistent sadness, loss of interest, and impaired functioning. Bipolar disorder involves significant mood swings, including mania or hypomania and depressive episodes. Psychiatric nurses play a vital role in assessing symptoms, providing emotional support, and educating patients and families. Effective management often combines pharmacotherapy with psychotherapy and lifestyle adjustments, aiming to enhance patients’ quality of life.
5.3 Anxiety Disorders and PTSD
Anxiety disorders, including generalized anxiety, panic disorders, and PTSD, are characterized by excessive fear, anxiety, or avoidance behaviors. PTSD specifically follows traumatic events, leading to intrusive memories and hyperarousal. Psychiatric nurses assess symptoms, provide reassurance, and implement evidence-based therapies like CBT. They also educate patients on coping strategies and lifestyle adjustments to manage symptoms and improve quality of life. Collaboration with mental health teams is essential for comprehensive care.
Treatment and Intervention Strategies
Treatment strategies blend pharmacological interventions, psychotherapy, and electroconvulsive therapy, tailored to individual needs. Nurses play a pivotal role in administering these therapies and ensuring patient-centered, evidence-based care.
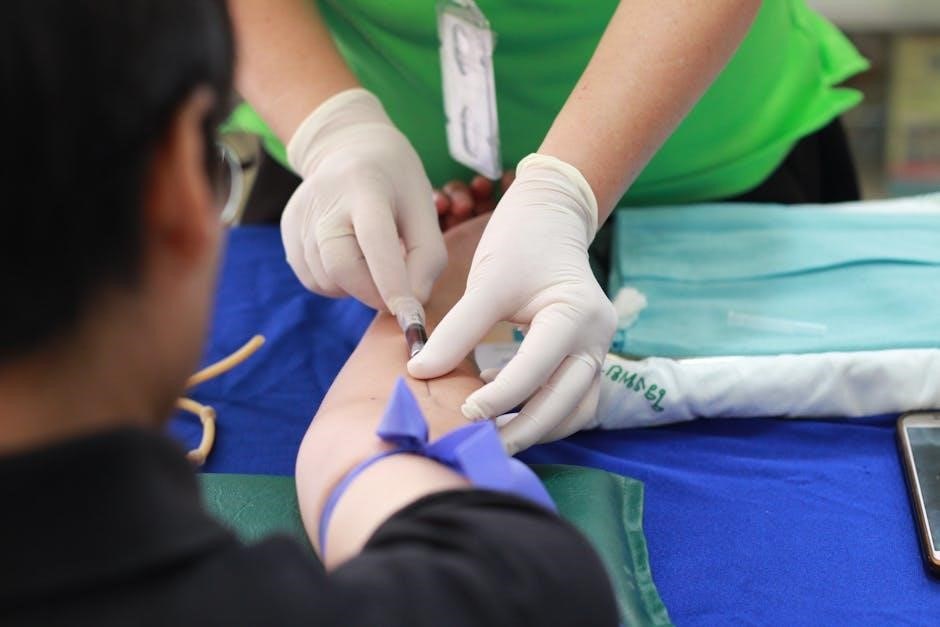
6.1 Pharmacological Interventions
Pharmacological interventions are cornerstone treatments in psychiatric nursing, focusing on medications like antipsychotics, antidepressants, mood stabilizers, and anxiolytics. These drugs help manage symptoms, balance neurotransmitters, and prevent relapses. Nurses play a critical role in administering medications, monitoring for side effects, and educating patients on adherence. Tailored pharmacotherapy plans ensure personalized care, enhancing patient outcomes and improving quality of life. Proper monitoring and education are essential for safe and effective treatment.
6.2 Psychotherapy Approaches
Psychotherapy is a core intervention in psychiatric nursing, focusing on evidence-based techniques to address mental health disorders. Approaches like cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), and family therapy are commonly used. These methods help patients identify thought patterns, improve coping strategies, and strengthen interpersonal relationships. Nurses play a vital role in facilitating these therapies, fostering a therapeutic alliance and promoting patient-centered care. Regular sessions and tailored interventions enhance emotional resilience and long-term recovery outcomes for individuals with mental health conditions.
6.3 Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (ECT) is a medical procedure used to treat severe mental health conditions, such as treatment-resistant depression, mania, and catatonia. It involves the application of a controlled electrical current to induce a seizure. ECT is highly effective for patients who do not respond to pharmacotherapy or psychotherapy. The procedure is performed under anesthesia and muscle relaxation. While controversial, ECT can rapidly improve symptoms, making it a lifesaving intervention for individuals in acute psychiatric crises. Modern advancements have minimized side effects, enhancing its safety profile.
Cultural Competence in Psychiatric Nursing
Cultural competence in psychiatric nursing involves understanding diverse beliefs, practices, and communication styles to deliver care that respects patients’ backgrounds, fostering trust and improving mental health outcomes.
7.1 Cultural Sensitivity in Patient Care
Cultural sensitivity in psychiatric nursing requires nurses to recognize and respect patients’ diverse backgrounds, beliefs, and values. This involves adapting care practices to meet individual needs, ensuring trust and rapport. Nurses should be aware of cultural differences in communication, emotional expression, and health practices. By fostering a nonjudgmental and inclusive environment, nurses can address stigma and promote equitable mental health care. Cultural sensitivity enhances patient engagement and improves overall treatment outcomes.
7.2 Understanding Cultural Influences on Mental Health
Cultural influences significantly shape mental health perceptions, expressions, and coping mechanisms. Nurses must recognize how cultural background, beliefs, and practices impact symptom presentation and treatment responses. Societal norms, family expectations, and stigma can influence help-seeking behaviors and therapeutic adherence. Understanding these factors is essential for providing culturally sensitive care, fostering trust, and improving outcomes. This awareness enables nurses to address diverse patient needs effectively and promote mental health equity.
7.3 Cultural Formulation in Assessment
Cultural formulation is a structured approach to understanding the cultural factors influencing a patient’s mental health. It involves identifying cultural identity, explanations of illness, cultural factors affecting the presentation, and treatment preferences. This framework enhances diagnostic accuracy, therapeutic alliance, and patient engagement. By integrating cultural insights, nurses can address diverse care needs, reduce disparities, and deliver person-centered interventions that respect individual beliefs and practices, ensuring comprehensive and culturally responsive mental health care.

Documentation and Reporting
Accurate documentation is crucial in psychiatric nursing, ensuring continuity of care, legal compliance, and effective communication among healthcare providers. It involves recording patient histories, treatment plans, and progress, adhering to confidentiality and ethical standards to support informed decision-making and accountability.
8.1 Effective Documentation Practices
Effective documentation in psychiatric nursing involves clear, concise, and organized recording of patient information, including histories, assessments, treatment plans, and progress. It ensures continuity of care, legal compliance, and accountability. Nurses should use standardized formats and avoid jargon to maintain clarity. Documentation must reflect patient-centered care, including mental status observations, interventions, and outcomes. Regular updates are essential to capture evolving patient needs and responses to treatment, supporting informed decision-making and collaboration among healthcare providers.
8.2 Reporting Changes in Patient Condition
Reporting changes in a patient’s condition involves timely and accurate communication of physical, emotional, or behavioral shifts. Nurses should use standardized tools to document and convey changes, ensuring clarity and consistency. This includes noting deviations from baseline assessments and the patient’s response to interventions. Effective reporting fosters collaboration among the healthcare team, enabling prompt adjustments to care plans. Clear communication is critical to prevent misunderstandings and ensure patient safety, particularly in acute mental health situations where rapid changes may occur.
8.3 Legal Implications of Accurate Documentation
Accurate documentation in psychiatric nursing is crucial for legal protection, as it serves as evidence of the care provided. Inaccurate or incomplete records can lead to legal claims of negligence or malpractice. Documentation must comply with regulations like HIPAA to ensure patient confidentiality. Clear and precise records protect both patients and healthcare providers, providing a defendable account of care. Thorough documentation also supports continuity of care and accountability, fostering trust in the therapeutic relationship.

Discharge Planning and Community Care
Discharge planning ensures a smooth transition to community care, involving family education, resource coordination, and ongoing support to promote long-term recovery and patient well-being.
9.1 Transitioning Patients to Community Care
Transitioning patients to community care involves creating personalized plans to ensure a smooth shift from inpatient to outpatient settings. Collaboration with community services, such as mental health clinics and support groups, is essential. Patients and families are educated on available resources, medication management, and follow-up care. This process promotes continuity of care, reduces readmissions, and supports patients in maintaining their mental health and independence in their community environments.
9.2 Family Education and Support
Family education and support are crucial in psychiatric nursing, as they empower relatives to understand mental health conditions and care strategies. Nurses provide information on symptoms, treatment options, and coping mechanisms. Families are encouraged to create a supportive environment, fostering resilience and recovery. Education helps reduce stigma and equips families to advocate effectively for their loved ones. This collaborative approach ensures patients receive consistent care and emotional support, enhancing their overall well-being and integration into community life.
9.3 Coordination with Community Resources
Coordination with community resources is vital for ensuring continuity of care post-discharge. Psychiatric nurses connect patients with services like mental health clinics, support groups, and social services. Collaboration between healthcare providers and community organizations facilitates a smooth transition, reducing hospital readmissions and promoting long-term recovery. Nurses also educate patients and families about available resources, enhancing their ability to access necessary support within their communities;
Professional Development and Support
Professional development and support are essential for psychiatric nurses to enhance skills, stay updated on best practices, and maintain resilience in their demanding roles.
10.1 Continuing Education for Psychiatric Nurses
Continuing education is vital for psychiatric nurses to stay updated on evidence-based practices, therapeutic interventions, and emerging mental health trends. It enhances clinical reasoning, cultural competence, and the ability to provide empathetic care. Nurses can engage in workshops, online courses, and conferences to expand their skills. This ongoing learning ensures they remain proficient in addressing complex patient needs and adhere to evolving healthcare standards, ultimately improving patient outcomes and professional growth.
10.2 Building Resilience and Avoiding Burnout
Building resilience is crucial for psychiatric nurses to manage the emotional and physical demands of their role. Engaging in stress management techniques, such as mindfulness and self-care practices, helps mitigate burnout. A supportive work environment and strong peer relationships also play a key role. Recognizing early signs of burnout, such as emotional exhaustion, is essential to maintain job satisfaction and provide effective patient care. Proactive strategies ensure nurses can thrive in their careers while delivering compassionate support to patients.
10.3 Peer Support and Mentorship Programs
Peer support and mentorship programs are vital for fostering professional growth and emotional well-being among psychiatric nurses. These programs provide platforms for sharing experiences, gaining insights, and developing coping strategies. Mentors offer guidance, helping nurses navigate challenges and enhance their clinical skills. Peer support reduces isolation, fosters collaboration, and promotes resilience; Such initiatives not only improve job satisfaction but also contribute to delivering high-quality, compassionate care to patients with mental health needs.